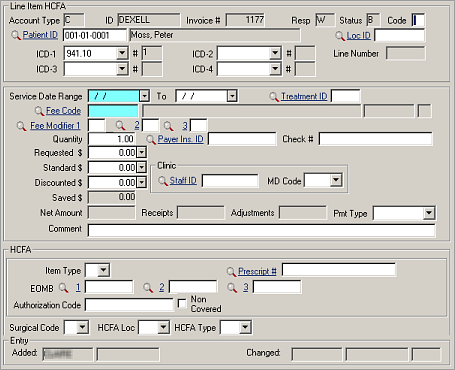
Provider of Services (Billing Provider) on a 1500 Claim Form (HCFA)
You must be certain that the Staff ID on the 1500 Claim Form is appropriate for the service provided. The ID that appears here is controlled by your global settings and the settings on an individual Medical Staff record. Globally, if you have checked Use Inj Provider for Billing on the screen, the primary physician on the injury will carry over for all injury-related invoices. If that setting is not checked, the staff person on the Treatment (Inj/Ill visit) record will be used. However, if the staff person on the Treatment record has some other ID in the Billing Provider field of the Medical Staff record, that other ID will be used.
Physical therapy/rehab bills will generally have to be on a separate invoice from other services, because there is only one space on the 1500 Claim Form for the name of the medical staff person, and all charges on that form are presumed to be related to that staff person. Specify PT in the Note field of the Invoice Header when the invoice is created so that the person doing the billing will assign subsequent physical therapy charges to the correct invoice. Also be certain that the Line Item record specifies the ID of the therapist (this will carry forward automatically from the Treatment record, if it is there). If it is blank on the Treatment record or the order, the Staff ID from the Injury will print on the 1500 Claim Form, which could cause it to be rejected.
| Label | Description |
|---|---|
| Service Date Range | Rather than a single date, 1500 Claim Form and UB Claim Form invoices require the beginning and ending dates of the period for which patient services are being billed. |
| MD Code | Code describing the role of
physicians:
|
| HCFA | |
| Item Type |
|
| Prescript # | Enter the prescription number if the facility is billing for a prescription dispensed by its own pharmacy. |
| EOMB | Explanation of Medical Benefits (three codes may be used). These codes are used from the Receipts/Adjustments screen to code why a charge was not paid. |
| Authorization Code | Enter code authorizing this charge (optional). This will fill automatically from the Treatment file, providing the treatment Authorization Code was carried to that file and the Treatment ID is specified. |
| Non-Covered | Check this box if you know that you won’t be paid for this expense (optional). |
| Surgical code |
|
| HCFA Loc | Location of service code for 1500 Claim Form (HCFA) billing, comes from the Fee table. |
| HCFA Type | Type of service code for 1500 Claim Form (HCFA) billing, comes from the Fee table. |