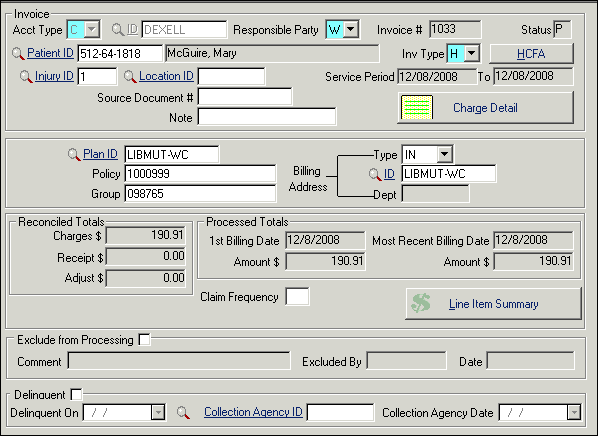
Invoices Screen
- Whether the bill is new or old (Status)
- Who is responsible for the bill (Account ID)
- Who will pay the bill (Responsible Party)
- Where the bill will be sent (Billing Address ID)
- What kind of invoice to print (Invoice Type)
- Who the bill is for (Patient ID)
- Which injury or illness the bill is for (Injury ID)
Before you post charges to a new invoice, you should always be certain that no suitable invoice already exists to which you could add your current charges. The goal should be to place as many charges as possible on one bill, except when billing insurance carriers or workers' compensation cases. In those instances, one visit/date of service per invoice is recommended.
| Label | Description |
|---|---|
| Buttons | |
| HCFA/UB/Standard | The top button changes based on the entry in the Invoice Type field: Standard, HCFA, or UB. HCFA (1500) and UB invoices require additional data to be entered on screens accessed with this button. Standard invoices do not require additional data, thus the button is disabled. |
| Charge Detail | This button shows a data screen view of the individual lines for this invoice. |
| Line Item Summary | The button on the bottom opens a grid view that displays all the charges, receipts, and adjustments for the invoice. On this view, you can optionally organize the lines so that the receipt is below the charge to which it applies. |
| Fields | |
| Acct Type | C Company or E Employee (patient). |
| ID | ID code of the company or patient account. |
| Resp Party |
Enter S , W , 1, or 2. Note: When the responsible party is
changed for an invoice, a new line item ($0 amount) is added to the invoice
detail for an auditing trail.
Once the responsible party is changed, for any invoice status other than Open, a (void) detail line is automatically added to explain what account previously contained the invoice. This provides an audit trail. This voided detail line will not show on reprinted invoices and does need to be reconciled.
|
| Invoice # | The program will automatically increment the number if you have set auto numbering "on" (the default) from the screen. This field may not be modified. |
| "Status:invoice;Billing:status" Status |
Program controlled, may show any of the following:
|
| Patient ID | A Worker's Compensation or other insurance invoice must have a Patient ID here, otherwise leave blank for multiple patients. Will be entered automatically if you used Orders related to an injury. The patient's name is displayed in the adjacent field. If there is a Patient ID, all transactions on this invoice must be for that patient. |
| Injury ID | Injury ID number (from Injury/Illness record, if applicable). Automatic if you are invoicing orders with an Inj ID. If there is an injury number, ALL transactions on this invoice must be for that injury. |
| Location ID | Automatically entered for a multi-location setup. This is the location for the invoice as a whole. If the charge details will come from more than one location, leave blank (erase if it auto-fills). |
| Source Document # | Enter the source document number that will identify this bill at the location that originated it (optional). |
| Note | Use to comment on what the invoice is for. This helps you identify the correct invoice for additional charges that may be added later. For example, enter June Screenings. |
| Invoice Type | (Required field) Enter H for HCFA (1500) invoices, U for UB, S for Standard. This controls additional options available for the invoice. |
| Service Period | Beginning and ending dates for the invoice. Required for UB Claim Form and 1500 Claim Form (HCFA) billing, defaults to today, and the ending date will expand automatically as you add line details with both service dates. |
| Plan ID | Benefit Organization Plan. Completed by program based on data in the Account and your entry in Resp Party field. Change if desired. |
| Policy | Completed by program if the number is available on the Account screen for this Resp Party . Change if desired. The policy # does not print on the invoice. |
| Group | Additional identification of insurance coverage. |
| Billing Address Type |
A billing address indicates the invoice will go to a different address than the responsible party's default address. The Type indicates which kind of ID:
|
| ID | Choose the appropriate Billing
Address ID for the specified Type.
Note: An entry in this field will
override the default mailing address for the Responsible Party.
|
| Dept | If the Billing Address ID Type is CD , enter the ID of the company department. |
| Reconciled Totals | |
| Charges | Total reconciled charges applied to this invoice. If the amount seems inaccurate, are any charges still waiting to be reconciled? Until that step is taken, they will not appear here. Charges entered through Orders can be set to reconcile automatically, but charges entered from the Invoice screen must be reconciled manually. |
| Receipt | Total reconciled receipts paid on this invoice. |
| Adjust | Total reconciled adjustments applied to this invoice. |
| Processed Totals | |
| First Billing Date + Amt | Program controlled, date and amount of first processing of this invoice. This date is the starting point for invoice aging. |
| Most Recent Date + Amt | Program controlled, date and current balance as of most recent processing. Used to determine date last billed for reprinting invoices with an outstanding balance. |
| Claim Frequency | Data element required when filing 837 claims electronically. Indicates whether the claim is initial (indicated by 1, the default entry), replacement (7), or voided (8); change as needed. |
| Exclude from Processing |
You can optionally delay an invoice that is not ready for billing by selecting this box. Deselecting this option allows the invoice to be processed. SYSTOC adds a detail record marked as Excluded or Included. Note: Clinics upgrading from older
SYSTOC versions and using this
option should obtain the revised
Preprocess Report that
correctly handles excluded invoices, available from the
SYSTOC Reports Department.
|
| Comment | Text field, activated when Exclude from Processing option is selected. Enter reason for exclusion, and update the explanation when including the invoice. The comment displayed on the invoice is stored in the new detail record. |
| Excluded By | Program controlled; the ID of the user who excluded or included the invoice. |
| Date | Program controlled; date the invoice was excluded or included. |
| Delinquent | Is the invoice delinquent according to clinic standards? Can be completed automatically. See Collections. |
| Delinquent On | Date the invoice became delinquent. |
| Collection Agency ID | Has this invoice been turned over to a collection agency? If so, select the ID of the agency from the list (links to the Attorneys/Collection Agencies file). |
| Collection Agency Date | Place the date of collection action in this field. |